What Effect Does Alcohol Have On A Skin Puncture If The
The information given hither supplements that given in Chapter two. Users of these guidelines should read Chapter two before reading the information given below. This affiliate covers background data (Department 7.1), applied guidance (Section seven.two) and illustrations (Section vii.3) relevant to capillary sampling.
Capillary sampling from a finger, heel or (rarely) an ear lobe may exist performed on patients of any age, for specific tests that require small quantities of blood. All the same, because the procedure is ordinarily used in paediatric patients, Sections seven.one.1 and vii.1.2 focus particularly on paediatric capillary sampling.
vii.1. Background information on capillary sampling
7.1.1. Choice of site
Adult patients
The finger is usually the preferred site for capillary testing in an adult patient. The sides of the heel are merely used in paediatric and neonatal patients. Ear lobes are sometimes used in mass screening or research studies.
Paediatric and neonatal patients
Selection of a site for capillary sampling in a paediatric patient is commonly based on the age and weight of the patient. If the child is walking, the child'south feet may take calluses that hinder acceptable blood flow. Table 7.ane shows the conditions influencing the choice of heel or finger-prick.
Table seven.ane
Weather influencing the choice of heel or finger-prick.
Specimens requiring a peel puncture are best obtained after ensuring that a baby is warm, as discussed in Section six.2.ii.
7.1.2. Selecting the length of lancet
Adult patients
A lancet slightly shorter than the estimated depth needed should be used because the pressure compresses the pare; thus, the puncture depth will be slightly deeper than the lancet length. In one study of 52 subjects, pain increased with penetration depth, and thicker lancets were slightly more painful than thin ones (67). However, blood volumes increased with the lancet penetration and depth.
Lengths vary by manufacturer (from 0.85 mm for neonates up to two.2 mm). In a finger-prick, the depth should not go beyond two.4 mm, so a ii.2 mm lancet is the longest length typically used.
Paediatric and neonatal patients
In heel-pricks, the depth should non go beyond ii.4 mm. For premature neonates, a 0.85 mm lancet is available.
The altitude for a 7 pound (iii kg) baby from outer skin surface to bone is:
-
medial and lateral heel – iii.32 mm;
-
posterior heel – ii.33 mm (this site should exist avoided, to reduce the risk of hit os);
-
toe – 2.xix mm.
The recommended depth for a finger-prick is:
-
for a child over 6 months and below 8 years – 1.5 mm;
-
for a child over viii years – two.4 mm.
Too much compression should exist avoided, considering this may crusade a deeper puncture than is needed to get good flow.
seven.i.3. Order of draw
With skin punctures, the haematology specimen is collected get-go, followed by the chemistry and blood banking concern specimens. This social club of drawing is essential to minimize the effects of platelet clumping. The order used for skin punctures is the reverse of that used for venepuncture drove. If more than than two specimens are needed, venepuncture may provide more accurate laboratory results.
7.1.4. Complications
Complications that can arise in capillary sampling include:
-
collapse of veins if the tibial artery is lacerated from puncturing the medial aspect of the heel;
-
osteomyelitis of the heel bone (calcaneus) (68);
-
nerve impairment if the fingers of neonates are punctured (69);
-
haematoma and loss of access to the venous co-operative used;
-
scarring;
-
localized or generalized necrosis (a long-term effect);
-
skin breakdown from repeated use of agglutinative strips (peculiarly in very young or very elderly patients) – this can be avoided if sufficient pressure is practical and the puncture site is observed afterwards the procedure.
7.2. Practical guidance on capillary sampling
7.2.1. Selection of site and lancet
-
Using the guidance given in Section vii.1, decide whether to utilise a finger or heel-prick, and decide on an advisable size of lancet.
-
Practice NOT use a surgical blade to perform a skin puncture.
-
Practice NOT puncture the skin more once with the same lancet, or use a single puncture site more than one time, because this can lead to bacterial contamination and infection.
vii.2.2. Process for capillary sampling
Adult patients
Set up the pare
-
Apply alcohol to the entry site and allow to air dry (come across Section 2.2.3).
-
Puncture the skin with one quick, continuous and deliberate stroke, to achieve a good catamenia of claret and to prevent the need to echo the puncture.
-
Wipe away the start drop of blood because information technology may be contaminated with tissue fluid or droppings (sloughing skin).
-
Avoid squeezing the finger or heel too tightly because this dilutes the specimen with tissue fluid (plasma) and increases the probability of haemolysis (sixty).
-
When the blood collection procedure is complete, apply firm pressure to the site to stop the bleeding.
Have laboratory samples in the correct gild to minimize erroneous test results
-
With skin punctures, collect the specimens in the guild beneath, starting with haematology specimens:
- –
-
haematology specimens;
- –
-
chemistry specimens;
- –
-
blood bank specimens.
Paediatric and neonatal patients
Immobilize the child
-
First immobilize the child by request the parent to:
- –
-
sit on the phlebotomy chair with the child on the parent'due south lap;
- –
-
immobilize the kid's lower extremities by positioning their legs around the kid's in a cross-leg design;
- –
-
extend an arm across the child's breast, and secure the child'south costless arm by firmly tucking it nether their own;
- –
-
grasp the child's elbow (i.due east. the skin puncture arm), and concur it deeply;
- –
-
employ his or her other arm to firmly grasp the child's wrist, holding it palm downwardly.
Prepare the skin
-
Gear up the skin as described above for adult patients.
-
Exercise Not use povidone iodine for a capillary skin puncture in paediatric and neonatal patients; instead, use alcohol, as stated in the instructions for adults.
Puncture the pare
-
Puncture the skin as described above for developed patients.
-
If necessary, take the following steps to improve the ease of obtaining blood past finger-prick in paediatric and neonatal patients:
- –
-
enquire the parent to rhythmically tighten and release the child's wrist, to ensure that in that location is sufficient period of blood;
- –
-
go on the child warm by removing as few clothes equally possible, swaddling an infant in a blanket, and having a mother or caregiver hold an infant, leaving but the extremity of the site of capillary sampling exposed.
-
Avoid excessive massaging or squeezing of fingers because this will cause haemolysis and impede blood flow (60).
Accept laboratory samples in the club that prevent cross-contamination of sample tube additives
-
As described higher up for adult patients, collect the capillary haematology specimen first, followed by the chemistry and blood bank specimens.
-
Make clean upwardly blood spills.
-
Collect all equipment used in the procedure, being careful to remove all items from the patient's bed or cot; to avoid accidents, DO Not exit annihilation backside.
Give follow-up care
There are 2 separate steps to patient follow-upwards care – data entry (i.eastward. completion of requisitions), and provision of comfort and reassurance.
Data entry or completion of requisitions
-
Record relevant information nearly the blood collection on the requisition and specimen label; such information may include:
- –
-
date of collection;
- –
-
patient name;
- –
-
patient identity number;
- –
-
unit of measurement location (plant nursery or hospital room number);
- –
-
test or tests requested;
- –
-
amount of claret collected (number of tubes);
- –
-
method of drove (venepuncture or skin puncture);
- –
-
phlebotomist'south initials.
Comfort and reassurance
Testify the child that you lot care either verbally or physically. A simple gesture is all it takes to go out the child on a positive note; for example, give verbal praise, a handshake, a fun sticker or a simple pat on the back.
A small amount of sucrose (0.012–0.12 one thousand) is condom and effective every bit an analgesic for newborns undergoing venepuncture or capillary heel-pricks (70).
Unsuccessful attempts in paediatric patients
Adhere strictly to a limit on the number of times a paediatric patient may be stuck. If no satisfactory sample has been collected after two attempts, seek a second stance to make up one's mind whether to make a further attempt, or cancel the tests.
7.3. Illustrations for capillary sampling
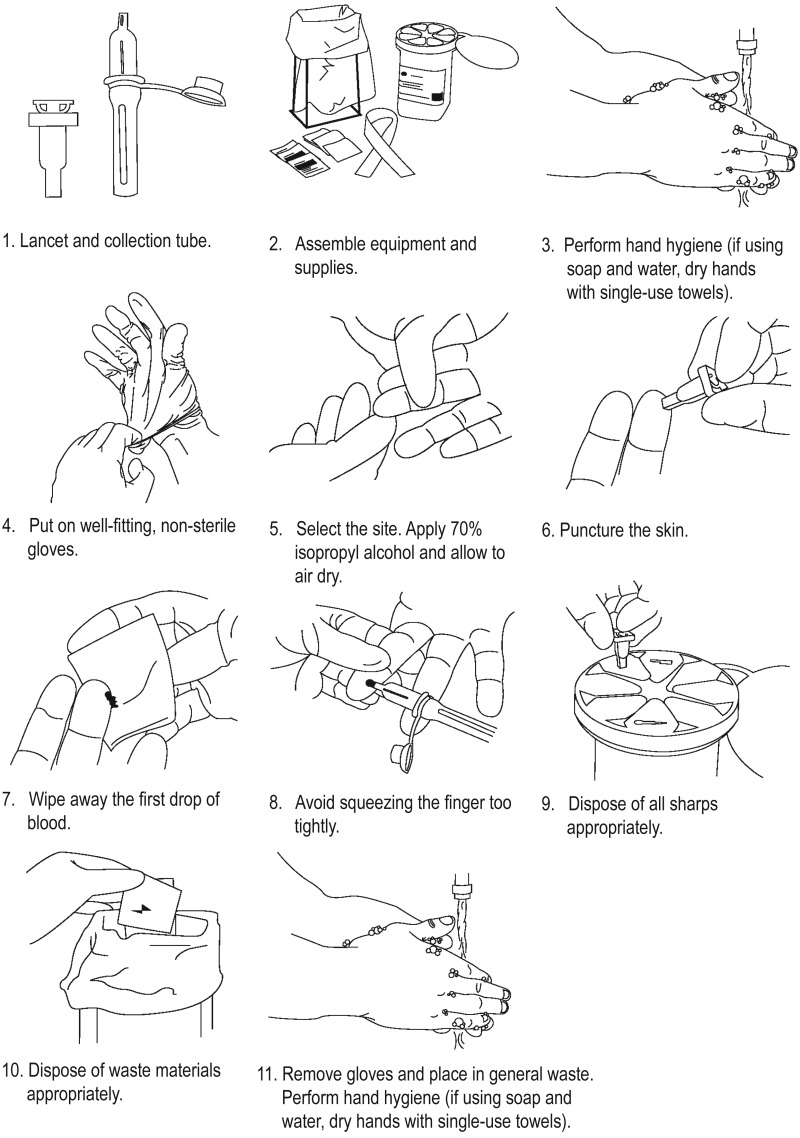
Effigy 7.one Capillary sampling
Source: https://www.ncbi.nlm.nih.gov/books/NBK138654/
Posted by: atenciomard1987.blogspot.com

0 Response to "What Effect Does Alcohol Have On A Skin Puncture If The"
Post a Comment